….Having just been released from the hospital for the second time in a week, I came home optimistic and ready to get back to work, scheduling more meetings with state health committee members, cleaning up my draft of the healthcare whistleblower bill I want to see passed, and setting up meetings with patients that wanted to help in the effort.
To my surprise….well, maybe not such a surprise…I was presented with yet another situation in which nurse(s) didn’t want to be affiliated with me because of what a Board of Nursing had to say about me several years ago, and the opinions of SEVERAL nurse bloggers who took it upon themselves to continue their assassination of my character not even knowing the full extent of the details involved in my case with Banner and the AZBON.
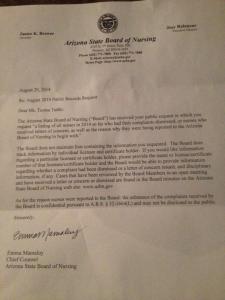
Its unfortunate. So here are the true facts— The AZBON LEFT OUT key witnesses that could have exonerated me and testified that I DID FOLLOW HOSPITAL POLICY when educating my patient. The AZBON left out that the Nurse Manager on my case Frank Fausto, lied when asked if I went up the chain of command to report a patient safety concern. The AZBON left out key information from the medical records that indeed shows I initiated a nurse order and has kept the medical record locked. The Arizona Board of Nursing has allowed nurses who have harmed patients, violated HIPPA, ammassed several aggravated DUI’s. diverted drugs, and even killed patients—back out there to practice with only the slap of a hand and a private reprimand.
Here are some more facts: I never hurt a patient in my life. I never under dosed or overdosed a patient. I never stole drugs. I never came to work intoxicated. I never left my posts. I never neglected or failed my patients.
Perfect? That was never a claim on my part. Ever. I was, in fact, just like you. Trying hard to toe the line in a corporatized environment that made me call into question my sense of morals and ethics every day. But social media and a board hell bent on painting a picture can do a whole lot to your life.
But the American Nurses Association wants you to have “moral courage.” They want you to stand up for your patients no matter what. What they don’t tell you about are the consequences to that.
Well, folks, here they are. The best part? You’re a criminal —for life. You don’t get to have a life anymore.
Truth be told, this nation never gave its people the option to choose those who have changed our way of being, our way of life, or our way of thinking—aside from a President or local government officials. No one handed out ballots for people like Martin Luther King or Rosa Parks or even Florence Nightingale. And before you start screaming to the masses, I am NOT comparing myself to them, ya dig?
Here’s the thing. People just saw a problem and spoke up. And did something. And didn’t stop doing something until the problem was fixed. I live by what is called a categorical imperative. I learned this in my undergrad years and never forgot it. It was the very heart of my nursing practice:
“You do for the sake of doing, not for what it will get you or where it will get you or how it will impact your personal circumstances or your comfort or your reputation—you do that which will benefit the greatest amount of people for the better.”
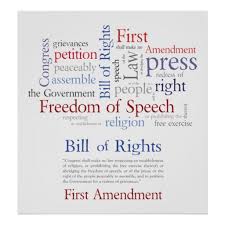
This was the spirit that kept me going up the chain of command to report a patient safety violation on the night of April 12, 2011. Its the same spirit that kept me fighting for my license and the same spirit that kept me fighting for the first amendment rights a board of nursing wanted to take from me.
It is the same spirit that has kept me fighting to protect the interests of nurses and patients today. My license may have been taken, but nurses are continuing to be harmed and patients continue to die TODAY.
Want to know my motive straight from me? There it is. So lets quit with the rumors. If I wanted to profit I would have finished the damn book by now and Lord knows I have enough material for three.
What matters to me is making sure not one more nurse loses their livelihood, their ability to provide for their families, their ability to adhere to a code of ethics they swore to uphold, impacting the rising number of senseless deaths each year that result from nurses unable to report unsafe situations or medical/surgical errors they know about.
You think you are in a state that is covered? You’d be surprised. I was. And its why I have been trying to fix it. I’m not in this for a license. I’m not in this for revenge. I’m in this because too many nurses and patients are getting hurt, and quite frankly, that IS HOW LAWS GET CHANGED. By people getting hurt. Or by a hole in the justice system.
Thankfully I don’t need permission or approval to get published. I don’t need permission to go see lawmakers or to make changes to current legislation, or to go speak before committee.
I don’t need permission or approval to be ME. And to be authentic and not watered down.
I don’t need permission to be part of a change movement.
I don’t need permission to help right what is so very wrong in our profession right now.
I don’t need to be “liked” to make change that benefits my colleagues and patients or the future of this profession.
I don’t need to be “perfect.”
All I “need” is the desire to do good, to change what is bad, and to help make it better so no one else goes through the same thing.
Want to fault me for that? Hold it against me? Judge me for it? Fine.
But in the same moment, ask yourself what you’ve done to not only walk the harried journey it takes to get there—but to accomplish the goals.
Until then, judge me not for the fact I spoke up and had ALOT of false things said about me and people who continue to HATE me.
Judge me for the fact I am a human being who is seeing other human beings get hurt and I’m just trying to do my part to make it right.
Fault me for that? Cool. Judge me for it? Look at yourself when you do it.
Try and make my voice useless and irrelevant– and my contribution to this profession I earned my right into ( I worked hard for that BSN and MSN just like you did) and sacrificed to be a part of?
Never.